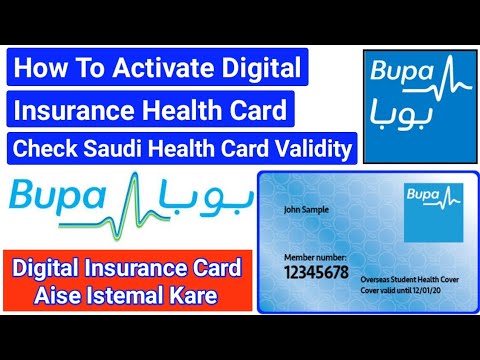
Many health insurance plans manage your prescription medications through a company called a Pharmacy Benefits Manager, or PBM. In some cases you will be issued a prescription insurance card that is separate from your medical insurance card. The back of your member ID card includes contact information for providers and pharmacists to submit claims. It also includes the member website and health plan phone number, where you can check benefits, view claims, find a doctor, ask questions and more.
If you forget or aren't sure what type of health insurance plan you have , you can find out on your BCBS ID card. If you have an HMO, your card may also list the physician or group you've selected for primary care. Determining whether a provider is in-network is an important part of choosing a primary care physician.
A member ID number and group number allow healthcare providers to verify your coverage and file insurance claims for health care services. It also helps UnitedHealthcare advocates answer questions about benefits and claims. Your member ID number and group number allow healthcare providers to verify your coverage and file claims for health care services. These numbers also help UnitedHealthcare advocates answer questions about your benefits and claims. The back of the member ID card may include phone numbers to connect with customer service, speak with a nurse and find behavioral health support.
It also includes contact information for providers and pharmacists to submit claims. The back of the member ID card includes the member website and phone numbers to connect with customer service, speak with a nurse and discuss behavioral health. It also includes contact information for providers and pharmacists to submit insurance claims. It's the identifier that lets healthcare providers verify the health insurance coverage and make the needed payment arrangements for the health care services provided. The managing entity is responsible for utilization management, claims processing, and ER admission/newborn notifications for assigned members.
Members are exempt from many of our special utilization management programs. See program descriptions to determine if HPC's members are excluded. All pharmacies use BIN and PCN numbers for processing prescription drug claims. The BIN number tells the computer database at the pharmacy which health insurance provider is to receive the claim for the prescription.
The PCN number is a second identifier that is used for routing claims. The Affordable Care Act requires all insurance plans offered by insurance companies and small employers to cover prescription medications. The policyholder, however, usually has to pay a part of the prescription costs. The Rx symbol on your insurance card tells you that your health insurance company pays for some or all of the prescription costs. Diagrams in the "Sample ID Cards" section of this chapter show how to quickly locate key coverage details and contact information. Your card contains key information about your health insurance coverage that is required when you need care or pick up a prescription at the pharmacy.
Keeping your card in a secure location will also help protect you from medical identity theft. At this point we can do nothing for the student other than to suggest that they call their parents and find out where the "missing card" or card information is. The students never enjoy hearing this and often state that their "other" pharmacy has always been able use this card! The type of health insurance plan you have is also indicated on your health insurance ID. It determines what medical provider you can go to and how you can get medical care.
If you have questions about which drugs are covered under your health insurance plan, contact the provider directly or consult its member materials. Anthem created a separate member toll-free number to direct pharmacy-related calls more efficiently to a dedicated Pharmacy Member Services team. Having this number means that pharmacy experts will help answer member questions about their prescription drug benefits.
It also will reduce customer effort in seeking help, which is a measure Anthem is tracking to assess member satisfaction. While a new pharmacy toll-free number will be listed, members will still be able to get their pharmacy questions answered through the general Member Services number. Specialty drugs are limited to a 30-day supply and you must get them from anin-network specialty pharmacy, so your benefits will apply to the prescription.
To encourage the proper use of prescription drugs, Blue Cross NC may restrict the amount of medicine your insurance plan covers. This may mean taking fewer pills each day without changing the total amount of medication. Most people with Blue Cross NC health insurance also have a drug plan to cover the drugs they get at their pharmacy. Each drug plan comes with a list that shows you what drugs are covered.
Your BCBS ID card has your member number, and in some cases, your employer group number. Your member number, also known as your identification number, is listed directly below your name. You'll need this information when receiving medical services at the doctor or pharmacy, or when calling customer service for assistance. If your group number is available, you'll find it directly below your member number.
Sometimes the medical insurance company does not cover prescriptions but prints the information of the prescription insurance company that does cover it on the same card. Sometimes the medical insurance company does not cover prescriptions but prints the information of the prescription insurance company in the top right corner of the issued card. Your insurance card can help you save money during your doctor's visits when you receive healthcare services and every time you go to the pharmacy. Every individual who is covered by health insurance has a unique member ID number, which is found on your insurance card.
It's a set of numbers that contains 5 to 12 digits and is listed under different headers such as member ID, ID, or membership #. A formulary is a list of prescription medications covered by your health insurance. Rx Grp is the group number assigned by a health insurance company to identify a member's group health plan. Your member ID card – like the example shown here – identifies you as a CareFirst member and shows important information about you and your covered benefits.
Each family member on your plan should have a card with their name on it. Make sure to always present your ID card when receiving services. If you don't have your physical card, you can view it on your smartphone through My Account.
Your member ID card may vary depending on your specific health plan and coverage. With those four numbers the pharmacy can properly submit a claim to the right insurance. When students bring their prescriptions to the WSSU Wellness Center Pharmacy, they are usually asked if they have their prescription insurance. Oftentimes the student produces a medical insurance card which does not contain the proper prescription insurance information. It could be your name or the name of your parents or spouse if you're covered by their health insurance plan. HMO – Health Maintenance Organization lets you choose the primary care provider that will coordinate your medical care.
You need to get a referral from your PCP if you need to see a specialist. It tells the pharmacy what type of insurance plan you have so they can look up the list of approved drugs, copays, and deductibles for your plan. These numbers allow your pharmacy or doctor's office to process claims through the right channels. These codes indicate what type of insurance you have, what type of drug coverage you're under, and where the claim needs to be submitted.
Some drugs may not be covered by your plan or may have a limited amount you can get with your plan. The Table of Drugs with Limited or No Coverage shows a sample listing. Our phones, keys, driver's licenses and credit cards are kept at our fingertips at all times. Those items are unique to each of us, and provide access to the things we need.
When it comes to healthcare services, that item is your Blue Cross Blue Shield ID card. If the insurance company covers prescription costs along with the medical coverage the letters Rx will be printed somewhere on the card. Some insurance companies include information about the prescription coverage on the insurance card. Show your insurance card every time you go on a doctor's visit or whenever you receive health services. POS – Point of Service lets you choose a primary care provider in your network.
You can use an in-network or out-of-network if you need to see a specialist at the time you need care. It tells the pharmacy whether your prescription is covered under your drug plan and if it is, how it would be paid. Each plan has its own list of prescription medications that are approved for reimbursement with coverage. If a medication isn't on the list under your plan, it's not covered. Also, this information is not intended to imply that services or treatments described in the information are covered benefits under your plan. Please refer to your Membership Agreement, Certificate of Coverage, Benefit Summary, or other plan documents for specific information about your benefits coverage.
Providers should verify member eligibility on emblemhealth.com/providers in addition to asking to see an ID card at each visit. No, these changes are mandatory, and they will help give members a smooth transition and make sure they can access their prescription drug benefits. The new ID card will reflect new, Anthem-owned BIN and PCN numbers and toll-free numbers for Pharmacy Member Services. These changes will help direct members and pharmacists to the right support, when they have questions about drug benefits.
2) Look for a capital letter or a capital letter/number combination after the "Rx" on your card.The letter will tell you which drug list, or formulary, your plan uses. The number gives information about the pharmacies in your network. Your BCBS ID card has important contact information to help you reach your BCBS company.
Look on the back of your card to find the phone numbers for customer service and eligibility questions. The plan name refers to the name of the plan or coverage you have from your health insurance provider. Cigna, Aetna, Kaiser, and Humana are some of the most common plan names. For instance, the CDPHP website has a section exclusively for updates to their covered drug list. In some cases, insurance cards show the Rx symbol along with a dollar or percent amount to show how much your insurer will pay for your prescription. Please see listfor specific drugs that are not covered.Medications used solely for weight lossPlease see member guide for coverage.
A non-formulary drug is one that isn't on your Blue Cross NC drug list. Doctors must confirm that you have tried a drug on your list first and that they were ineffective or harmful to you. Also, medication-specific clinical criteria must be met before approval . Our drug search tool shows the restricted drugs our members use most, and the details your doctor or provider must send us to get them approved. Quality Care That's Right for YouWhether you need a routine check-up or a specialty procedure, you want the best care you can find. BCBS recognizes doctors and hospitals for their expertise and exceptional quality in delivering care.
Learn more about our Total Care and Blue Distinction® Specialty Care designation programs and find a designated doctor or hospital that meets your needs. Unfortunately, new health care fraud and abuse schemes are constantly occurring. You can help protect yourself and your family by staying informed. PPO – Preferred Provider Organization lets you visit any medical professional without the need for a referral from your primary care provider.
If you're not sure what your Rx Grp is, contact the customer service phone number listed on the back of your ID card. When the pharmacist types your Rx BIN into their database, they'll know which insurance company will pay for your prescription. Any information provided on this Website is for informational purposes only. It is not medical advice and should not be substituted for regular consultation with your health care provider. If you have any concerns about your health, please contact your health care provider's office.
Effective July 1, 2020, GHI PPO City of New York members will use K-IDs. Empire BCBS will adopt the same K-ID but will only use and display the first 9 digits on their member ID cards. City of New York members who are also eligible for Medicare benefits will have member ID cards issued to all family members individually in compliance with CMS regulations. Anthem is updating pharmacy information on their ID cards to give members a better experience at the drugstore.
Your clients will receive a new ID card at renewal, starting in October 2018 and continuing through April 1, 2019. Groups scheduled to renew between May 2019 and October 1, 2019 will get a new ID card off renewal in the months of February and March 2019. Blue Cross and Blue Shield of North Carolina does not discriminate on the basis of race, color, national origin, sex, age or disability in its health programs and activities.
Learn more about our non-discrimination policy and no-cost services available to you. Your BCBS ID card may include a list of the co-pay amounts you can expect to pay for common services, like a doctor's visit or trip to the emergency room. The Blue Cross Blue Shield System is made up of 35 independent and locally operated companies. If you need more information about your insurance or if you can't find the information you need, you should call your health insurance provider right away.
What Does Rx Mean On Insurance Card Some insurance policies do not use a tiered system, but instead, assign each drug a copayment amount. In this case, the copayment amount should be listed on your card or your member information packet. Because your insurance will only pay for drugs included in your plan's formulary.
A doctor's office could also use this information to verify your eligibility for coverage before providing services. We recommend contacting your health insurance provider to confirm your Rx BIN. All members receive their own personal member identification card. Our New York City GHI PPO members are issued two ID cards, one from EmblemHealth and one from Empire BlueCross BlueShield . Physical cards are mailed to members and are available virtually from the Member Management Eligibility look-up results in the provider portal. Most members (about 85%) will get new cards during their plan's regular renewal period, even if they don't have any changes to their benefits at that time.





















No comments:
Post a Comment
Note: Only a member of this blog may post a comment.